Neuro & Brain
Craniotomy Treatment
Skull Surgery
Like any other part of the body, the brain is susceptible to bleeding, infection, trauma and other forms of damage. This damage or alteration in brain function sometimes requires brain surgery to diagnose or treat these problems.
What is Craniotomy?
The Craniotomy is a surgery used to cut a bony opening in the skull. A part of the skull, (called as the bone flap) is removed to access the brain underneath. A craniotomy may be small or large depending on the problem of the patient. The surgeon uses special tools to remove the section of bone called the bone flap. After the brain surgery, the surgeon replaces the bone flap and attaches it to the surrounding bone with the help of small titanium plates and screws. If the part of the skull bone is removed and is not replaced right away, it is called craniectomy. This is performed if the swelling is likely to occur after brain surgery or if the skull bone flap can't be replaced for other reasons. After a few weeks to months, the patient may have to follow-up surgery called a cranioplasty. During a cranioplasty, the missing piece of the skull will be replaced with your original bone, a metal plate, or with a synthetic material.
Why do I need Craniotomy?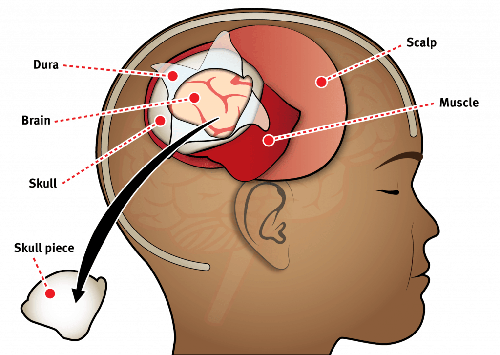
Doctors may perform a craniotomy for a variety of reasons, these reasons may include:
- Diagnosing, removal, or treating brain tumor.
- Clip or repairing an aneurysm.
- Removal of blood or blood clots from a leaking blood vessel.
- Removing an arteriovenous malformation. This is an abnormal mass of blood vessels
- Draining an infected pus-filled pocket (abscess).
- Repairing skull fractures.
- Repairing a tear in the membrane lining of the brain.
- Relieving pressure within the brain (intracranial pressure) by removing damaged or swollen areas of the brain that may be caused due to traumatic injury or stroke.
- Treating epilepsy. This is a neurological condition which involves the brain that makes people more likely to have seizures.
- Implanting stimulator devices for treating movement disorders such as Parkinson's disease or a type of movement disorder called dystonia
- Treating hydrocephalus
Do’s and don’ts before the surgery
Before the Surgery:
- The Patient may be scheduled for presurgical tests (e.g., blood test, electrocardiogram, chest X-ray) several days before the surgery takes place.
- The Surgeon must be correct medical history (allergies, medicines/vitamins, bleeding history, anesthesia reactions, and previous surgeries) by the patient.
- The patient must discuss all medications (prescription, over-the-counter, and herbal supplements) that he/she is taking.
- All non-steroidal anti-inflammatory medicines (Naprosyn, Advil, Motrin, Nuprin, Aleve, etc.) and blood thinners (Coumadin, Plavix, etc.) must be avoided 1 to 2 weeks before surgery as directed by the doctor.
- Additionally, smoking, chewing tobacco, and drinking alcohol must be prohibited 1 week before and 2 weeks after the surgery because these activities can cause bleeding problems.
- No food or drink is permitted past midnight the night before surgery takes place.
Morning of surgery
- Shower with the help of antibacterial soap. Wear loose fitting and freshly washed clothes.
- Wear flat-heeled shoes having closed backs.
- If the patient has been given instructions to take regular medication the morning of surgery, do so with small sips of water.
- Remove any make-up, hairpins, contacts, body piercings, nail polish, etc.
- Leave all valuables and jewelry at home.
- Patient must have a list of medications with dosages and the times of day usually taken.
- Patient must have a list of allergies to medication or foods.
- Arrive at the hospital 2 hours prior to the scheduled surgery time to complete the necessary paperwork and pre-procedure work-ups.
Procedure for Craniotomy
The Human craniotomy is usually performed under general anesthesia but it can be also performed with the patient awake using a local anesthetic. This procedure generally does not involve significant discomfort for the patient. A craniotomy will be preceded by an MRI scan which provides an image of the brain that the surgeon uses to pinpoint the precise location for bone removal and find an appropriate angle of access to the relevant brain areas. The amount of skull that needs to be removed depends on the type of surgery being performed by the surgeon. The bone flap is mostly removed with the help of a cranial drill and then it is replaced using titanium plates and screws or another form of fixation like wire, suture, etc. If the host bone does not accept its replacement an artificial piece of skull, often made of PEEK, is substituted. The patient may experience a headache or even nausea after surgery. Medication will help in controlling these symptoms. Depending on the type of brain surgery, steroid medication (to control brain swelling) and anticonvulsant medication (to prevent seizures) may be given to the patient. The length of the hospital stay may vary, from only 2–3 days or 2 weeks depending on the surgery and any complications.
Risks involved during Craniotomy
All treatments and outcomes may vary from patient to patient. Complications such as infection, nerve damage, blood clots, blood loss, bowel and bladder problems, along with complications associated with anesthesia, are some of the potential risks of spinal surgery.
Complications associated with a craniotomy may include
- Stroke
- Seizures
- Brain swelling, which may require another craniotomy
- Nerve damage which results in muscle weakness or even paralysis
- Cerebrospinal fluid leak
- Mental impairment
- Permanent brain damage and associated disabilities
The following complications are rare and are only related to specific places in the brain
- Memory problems
- Speech difficulty
- Paralysis
- Abnormal balance or coordination
- Coma
Recovery
The patient will be given a follow-up appointment for 10 to 14 days after surgery. The recovery time may vary from 1 to 4 weeks depending on the underlying disease being treated and the patient’s general health. Full recovery may even take up to 8 weeks. Walking is a good way to begin increasing a person activity level. One mustn’t overextend himself/herself, especially if that person is continuing treatment with radiation or chemotherapy. One must ask his/her surgeon when he/she can return to work.
Introduction about Craniotomy Treatment in India
Craniotomy is an operation where a part of the skull is temporarily taken off to access the brain. This particular surgery is often employed to manage other diverse forms of brain conditions such as head injuries, cerebrovascular aneurysms, and cerebral tumors. Due to advances in craniotomy surgery, India has become now a preferred destination for affordable, quality neurosurgery care.
About Craniotomy Treatment
A craniotomy is a serious operation in which a portion of the skull of the individual is cut off to reveal the brain. Craniotomy surgery is used to treat a variety of brain disorders, including:
- Brain tumors
- Stroke causing brain edema
- Epilepsy
- Blood clots in the brain
- Brain aneurysms
- Hemorrhage
- Skull fractures
Types of Craniotomy
- Meningioma Craniotomy: Meningiomas are tumours located in the meninges – the protective covering of the brain and spinal cord. Meningioma Craniotomy is performed especially for the removal of these tumours with the aim of achieving meningioma.
- Middle Fossa Craniotomy: Middle Fossa Craniotomy is a little of a different category of craniotomy that is done for any condition that is close to the temporal bone affecting balance and hearing, including acoustic neuromas.
Need for the Treatment
- Craniotomy surgery is a very important procedure when it comes to management of severe brain disorders that include tumor, aneurysm and trauma.
- It is required when conservative management of these conditions does not work.
-
For the patients diagnosed with meningiomas, meningioma craniotomy is mandatory since it relieves headache and other symptoms, such as seizures.
-
Middle fossa craniotomy is also used in the removal of acoustic neuromas, avoids damaging the nerve and enhances the neurological quality.
Symptoms of Craniotomy
Conditions that lead to a craniotomy often exhibit specific symptoms, including:
- Severe headaches
- Seizures
- Nausea and Vomiting
- Vision problems
- Difficulty with balance
- Cognitive changes
- Weakness
- Speech difficulties
After the craniotomy surgery, patient may experience certain symptoms, including:
- Inflammation and tenderness of the area surrounding the surgical cut.
- Fatigue or drowsiness.
- Lasting confusion or memory troubles that are temporary.
- Poor or clumsy mobility during the recovery period.
Risk Factors of Craniotomy Treatment
Of course, any surgical operation works with some potential dangers, and a craniotomy is not an exception. On the same note, craniotomy surgery can potentially carry out remarkable and life-saving treatment of disorders affecting the brain’s activity; however, there are conditions that facilitate the likely emergence of problems:
- Infection of a site that is the surgical site or an infection in the brain.
-
Bleeding within the brain
-
Brain swelling
-
Seizures
-
There may be more potassium or other blood clots causing a stroke after some craniotomy has been made
-
Neurological changes that include weakness, blurred vision, speech difficulties, or memory impairment.
Causes of Craniotomy
This type of surgery may be carried out when diseases cannot be effectively managed by other corresponding methods namely injury or congenital deformities. The following are the primary causes a craniotomy might be required:
- Brain tumors
- Brain aneurysms
- Traumatic Brain Injury
- Epilepsy
- Brain Hemorrhage
- Stroke
- Neurological Disorders
Facilities and Services offered for International Patients for Craniotomy Treatment
India’s hospitals have specialized multiple treatments for those international patients who want to avail the latest medical facilities like craniotomy surgery. They include special international patient officers, medical visa facilitation, medical treatment packages, airport pick-up & drop, language translation, travel and executive assistance, telemedicine and preliminary consultation, patient’s advocate, consulting in second opinion, offering standard premium medical care, post-surgical care, & rehabilitation, appealing food & cultural, preferences, support in billing & insurance, and medical tourism & wellness services.
Process of Craniotomy Treatment
Pre-craniotomy treatment
The pre craniotomy treatment carries a pivotal role to ascertain the effectiveness, non-risk element and a successful craniotomy. It includes several processes in assessing the result of the patient and for the preparation of the patient for surgery and several sub-steps about the surgery:
- Medical assessment as well as neurological assessment is done during consultation and diagnosis.
-
The imaging & diagnostic model includes MRI, CT Scan, Angiography and EEG.
-
Surgical Planning
-
Blood test, electrocardiogram and chest X-Ray are among the preoperative tests that are done.
-
Medical Clearance
Diagnostic Tests for Craniotomy
The craniotomy treatment diagnosis in India is quite a lengthy process, with many tests and evaluations done in order to properly categorize the disorder of the brain, as well as to determine whether surgery is indeed needed. That is, finding out the issue that really needs to be addressed, assessing its implications for the overall situation, and changing the approach to the surgery as a result. The usual diagnostic procedures carried out before to a craniotomy are listed below:
- Brain Imaging Tests such as MRI’s and CT scans.
-
Cerebral Angiography depicts the blood flow within vessels of the brain and is important in diagnosing aneurysms.
-
Electroencephalogram detects issues like seizure or epilepsy.
-
Cardiac and Pulmonary tests like EKG, Chest X-ray and Pulmonary Function Tests.
Craniotomy Treatment
A craniotomy is a surgical technique whereby the surgeons remove the bone of the skull to get to the brain. It is believed that two and a half hours might elapse during the undertaking. The whole procedure consists of:
- Preparation: Patient removes all rings or other items on her hands and wrists, is gowned for surgery; IV line and catheter are initiated; and the patient is put on the operating table for brain surgery. Anaesthesiologist control the rate of pulse, blood pressure, respiratory process and blood oxygen level.
-
Cleaning and shaving: The surgeon then uses an antiseptic solution to wash the skin and is sure to shave the hair around the area of the cut.
-
Incision: Surgically, an incision is made on the skin. The kind of craniotomy depends on location of the skin incision done to expose the head of the skull.
-
Drilling: A small hole, or several holes which are small in size, are made on the patient’s skull by the surgeon.
-
Bone Flap Removal: The bone flap is then removed from the skull using a saw where the surgeon incubates the area often where the bone flap is required. Finally, some surgeons remove the bone flap at the end of the surgery, although it may be used to rewrite the skull.
-
Brain exposure: The head is covered by a tough layer of skin known as dura mater which the surgeon first separates before any operation on the brain.
-
Brain surgery: In a surgical procedure, depending on the reason why the operation is required, the surgeon works on the brain.
-
Closure: The bone flap is then replaced by the surgeon and held in position by use of wires, screws, plates or stitches. After that, the surgeon stitches the testicular incision and also repositions all the abnormal placed muscles or tissues cut during the surgery.
Post-craniotomy treatment
Post-craniotomy treatment includes:
-
Monitoring: Patients’ postoperative hours vital signs and neurological status are monitored in the operative care room and later in the Intensive care unit.
-
Pain management: A physician prescribes medicines that are intended to help patients reduce discomfort which they feel.
-
The patients’ heads are positioned slightly higher than the rest of the body in order to reduce inflammation.
-
Wound care
-
Deep breathing: It is advised that patients go through breathing exercises for the sake of preventing respiratory problems as well.
-
Patients’ needs are satisfied, patients’ phobias are alleviated.
-
After recovery, the patients must have appointments with their doctor frequently.
-
Patients are allowed only bed rest in order to avoid those activities which can make them tired.
-
Patients need to take more balanced diets.
Success Rate of Craniotomy Treatment
In India, craniotomy surgery success is normally high, post-surgical death rate is almost negligible. Craniotomy surgery has a high surgical success rate of 96-48% depending on size of tumour and condition of the patient.
India’s Best Hospitals for Craniotomy
-
Fortis Memorial Research Institute, Gurgaon
-
Apollo Hospital, Mumbai
-
Wockhardt Hospital, Mumbai
-
Indraprastha Apollo Hospital, New Delhi
-
Max Super Speciality Hospital, New Delhi
-
Artemis Hospital, Gurgaon
-
Medanta - The Medicity, Gurgaon
India’s Best Doctors for Craniotomy
-
Dr. Mazda Turel
-
Dr. Sanjay Mongia
-
Dr. Sandeep Vaishya
-
Dr. Suresh Sankhla
-
Dr. Aditya Gupta
-
Dr. Sudheer Tyagi
Why choose Get Well Go for Craniotomy Treatment in India?
Several factors that Get Well Go using craniotomy treatment has can make a number of impacts that can enhance a patient's experience and outcome. The several factors are:
-
Get Well Go has very skilled and knowledgeable neurosurgeons that perform craniotomy surgery.
-
Get Well Go integrates hospitals that possess adequate technologies in neurosurgery, and the required medical equipment.
-
Care given before and after the operation.
-
To accommodate International patients.
-
Cost-effective treatment.
-
Positive Patient Testimonials.
-
Ongoing Support.
Conclusion
Craniotomy is a surgical procedure that seeks to remove part of the skull to access a particular part of the brain that requires treatment as a result of tumor formation, aneurysms and other neurological problems. This is why it is essential to determine pathologies in this organ and in the human body in general. Awake neurosurgery is a relatively new model for the neurosurgical operations that are performed on a conscious patient. In this technique, functional preservation can be made with low dependency on follow up surgeries and fast rates of regeneration. These techniques as cortical and awaked neurosurgery introduce the opportunities to rescue function, revive invasive procedures, and improve the beneficial result. However, there are; patient anxiety, intraoperative complications and postoperative effects as the negative factors. Thus, the knowledge of those risks should be transferred to the patients in order they make the right decisions for their health as much as possible.
FAQs
1. In most cases how long does it take to have a craniotomy??
- An awake craniotomy with stimulation typically lasts 5-7 hours, a craniotomy without stimulation takes 3-5 hours.
2. How long does this whole process of recovery take?
- A full restoration of locomotor function may require several weeks, and time to return to walking can vary between the range of 1 and 4 weeks.
3. How should I proceed following a craniotomy?
- Your doctor should prescribe prophylactic pain management and you should avoid aspirin and all other anticoagulants. As for lung infections, you should continue with your breathing exercises and refraining from irritants and upper respiratory diseases
4. When should I go to my physician?
- You should contact your physician if you have a fever, the pain is severe or increasing, or your surgical area fails to heal as expected.
TREATMENT-RELATED QUESTIONS
GetWellGo will provide you end-to-end guidance and assistance and that will include finding relevant and the best doctors for you in India.
A relationship manager from GetWellGo will be assigned to you who will prepare your case, share with multiple doctors and hospitals and get back to you with a treatment plan, cost of treatment and other useful information. The relationship manager will take care of all details related to your visit and successful return & recovery.
Yes, if you wish GetWellGo can assist you in getting your appointments fixed with multiple doctors and hospitals, which will assist you in getting the second opinion and will help you in cost comparison as well.
Yes, our professional medical team will help you in getting the estimated cost for the treatment. The cost as you may be aware depends on the medical condition, the choice of treatment, the type of room opted for etc. All your medical history and essential treatment details would be analyzed by the team of experts in the hospitals. They will also provide you with the various types of rooms/accommodation packages available and you have to make the selection. Charges are likely to vary by the type of room you take.
You have to check with your health insurance provider for the details.
The price that you get from GetWellGo is directly from the hospital, it is also discounted and lowest possible in most cases. We help you in getting the best price possible.
No, we don't charge patients for any service or convenience fee. All healthcare services GetWellGo provide are free of cost.
Top Doctors for Neuro & Brain
Top Hospitals for Neuro & Brain
Contact Us Now!
Fill the form below to get in touch with our experts.



%20Joy%20Dev%20Mukherji.jpg)



